Case of the Month - AUGUST 2024
CASE
A 52-year-old male presents with a decade of known internal and external hemorrhoids with intermittent week-long episodes of hematochezia and BRBPR every 2-3 months, resulting in anemia. The patient underwent rubber band ligation in 2016, and his most recent colonoscopy in 2024 demonstrated engorged circumferential Goligher grade I-II hemorrhoids with stigmata of bleeding. He was referred to IR for consideration of hemorrhoid artery embolization.
The Goligher Grading system describes hemorrhoid severity.
Grade 1: no prolapse
Grade 2: prolapse upon bearing down with spontaneous reduction
Grade 3: prolapse requiring manual reduction
Grade 4: prolapse with inability to reduce manually.
The best candidates for HAE have internal hemorrhoids, grade 1 with hemorrhagic symptom predominance, or grade 2/3 with prolapse. Patients with grade 4 hemorrhoids are not ideal candidates as HAE may not improve significantly prolapsed or thrombosed hemorrhoids.
The IMA typically arises at the level of L2-L3 and gives rise inferiorly to the superior rectal artery (SRA). The SRA then divides into left and right branches around the level of S3, which may divide further into anterior and posterior branches. Assuming conventional anatomy, there are thus 4 main contributing sub-selective hemorrhoidal vessels (left anterior, left posterior, right anterior, and right posterior) divisions of the SRA. The left colic artery (ascending and descending branches) arises proximally to the sigmoid arteries, which can less frequently supply hemorrhoidal arteries.
Here is an image from the digital subtracted IMA angiography of this patient: (note the spiral hemorrhoidal arteries inferiorly, red arrows):
Here is an example of a run from a sigmoid artery (left image) This was NOT treated in this case as it did not feed any hemorrhoidal artery and instead supplies sigmoid colon. The right image shows the vascular anatomy in this region. IMA – inferior mesenteric (L2-L3); LC – left colic; SH – superior hemorrhoidal (superior rectal); MC – middle colic (filled retrograde); ABr – ascending branch, left colic; DBr – descending branch, left colic; S – sigmoid.
CT angiography can be helpful in mapping the topology of the inferior mesenteric artery/superior rectal artery and, if contributory, the internal iliac/middle rectal artery. Blushing of the hemorrhoidal plexuses may also be seen, which can signal the presence of contributing hemorrhoid arteries (likely below the level of the pubic symphysis).
This hemorrhoidal arterial supply is demonstrated in approximately 66.5% (about 2/3) of HAE cases. Unilateral SRA hypertrophy with contralateral MRA involvement is seen in about 27% of cases. Currently, sub-selecting the MRA is not necessarily indicated if bilateral SRA hypertrophy is seen on DSA and the MRA is not visualized on post-embolization DSA.
There is currently no definitive evidence regarding a standardized optimal embolic regimen, however, most evidence suggests using a combination of coils and particles (at least 500-700 um) (Zakharchenko et al). Coils alone and particles alone are also safe and effective in the setting of HAE. Continued longitudinal monitoring of symptom recurrence (i.e., via patient-reported outcome measures), need for re-treatment, and adverse effects is underway to continue to identify an optimal embolic strategy.
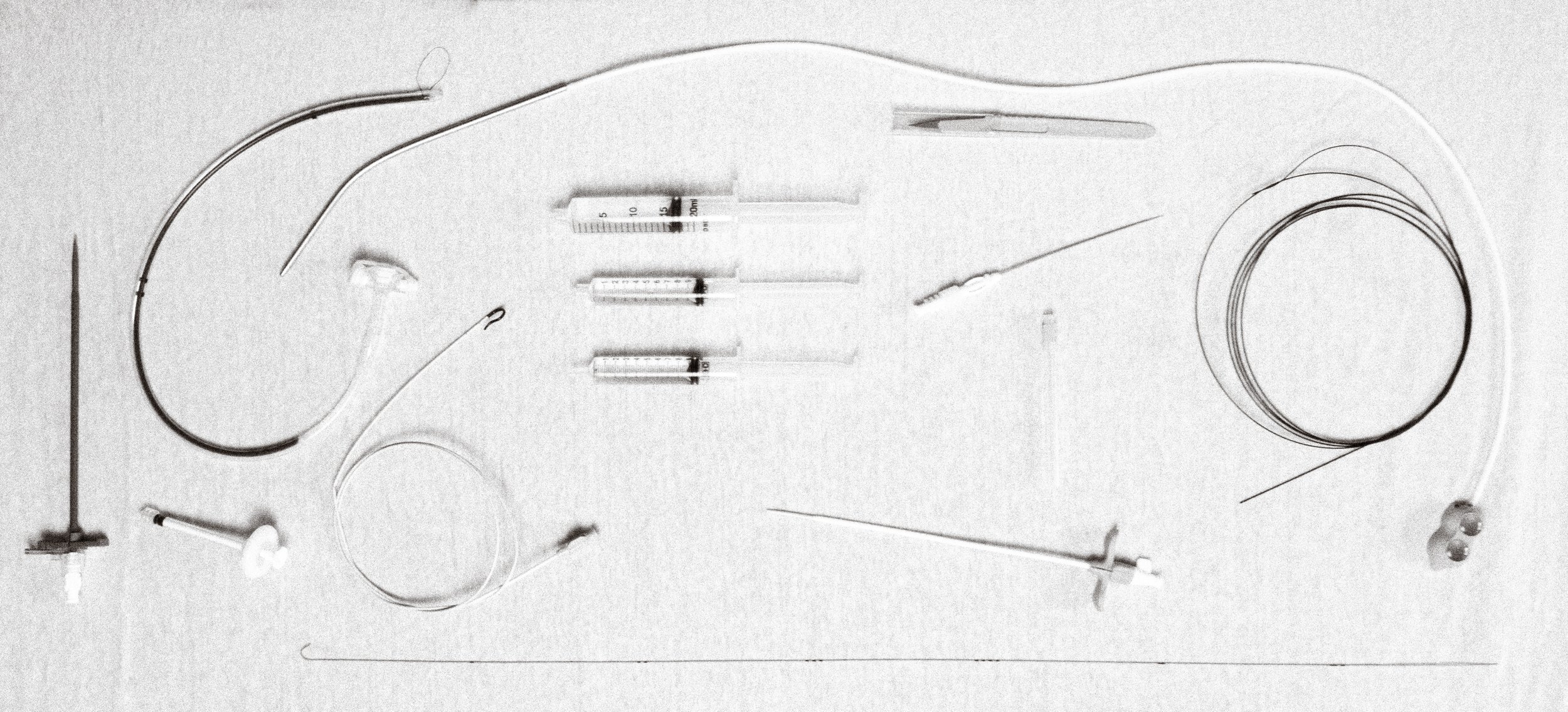
Depicted below is a post-embolization run from the distal left anterior superior rectal artery using 500-700 um particles packed with 2 mm coils (left image) as well as a different case with microcoils used to occlude the major branches.
LEARN MORE
Zakharchenko et al. (2016). Describes the “Emborrhoid Technique.”
Bagla et al. (2023). Outcomes from Hemorrhoid Centers (multidisciplinary centers)
BackTable Podcast of Hemorrhoid Embolization with Dr. Alex Pavidapha
Case contributed by Drs. J.C. Panagides, Benjie Smith, and Amanda Rigas from Stanford University






