Case of the Month - September 2024
CASE
A 72 year old man presented with lower urinary tract symptoms including urinary frequency, urgency, urge incontinence, weak stream, and straining. He started finasteride and tamsulosin but had minimal improvement with 6 months of conservative management. CT scan revealed the patient’s prostate volume was 113 mL, and his PSA was 2.0.
There is no upper limit on the maximum prostate size for PAE. Prostatic urethral lift, transurethral resection of the prostate, and water vapor thermal therapy are some of the options for prostates <80 mL in size according to guidelines from the American Urological Associate (AUA). Prostate artery embolization as well as simple prostatectomy, holmium laser enucleation of the prostate (HoLEP), and aquablation are options for large and very large prostates. Notably, the AUA guidelines were updated in 2023 and were significant for their inclusion of prostate artery embolization as a treatment option for lower urinary tract symptoms related to BPH.
This patient desired minimally invasive treatment for his symptoms and was referred for PAE.
According to the 2019 Society for Interventional Radiology position statement, the indications for PAE include moderate to severe lower urinary tract symptoms related to BPH, chronic urinary retention related to BPH as a means to achieve catheter independence, and hematuria of prostatic origin as a means to achieve cessation of bleeding.
Indications for PAE for lower urinary tract symptoms:
International Prostate Symptom Score (IPSS) > 12-14. The IPSS is a score derived from a questionnaire about patients’ voiding symptoms.
Prostate Volume >40 mL. There is no upper limit on prostate size for PAE.
Urodynamic studies with peak urinary flow rate (Qmax) <12 mL/s, which is predictive of bladder outlet obstruction.
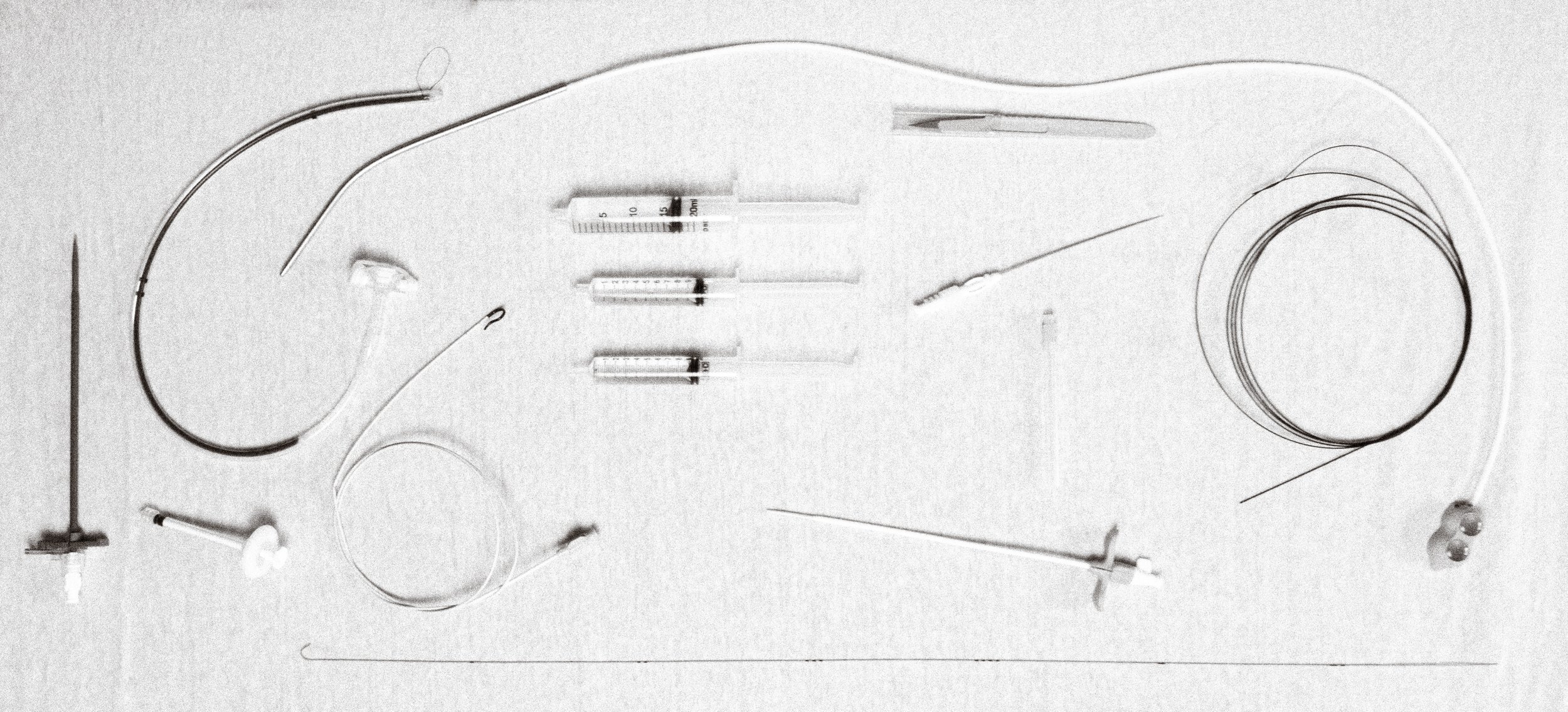
The patient presented for PAE. Access to the right femoral artery was obtained. An Omni flush catheter and Bentson wire were used to go over the iliac bifurcation, and a Roberts Uterine Catheter (RUC, now renamed RBT) was used to select the left internal iliac artery. DSA was performed.
Typically, the obturator artery is also visible, however it was replaced to the external iliac artery in this patient. A mnemonic that can be helpful to remember the branches of the internal iliac artery is PROVISO (internal Pudendal artery, middle Rectal artery, Obturator artery, Vesical Inferior and vesical Superior arteries, which are best visualized with an ipsilateral Oblique view). The inferior vesical artery and prostatic artery branches typically arise from a common trunk.
Prior to embolizing, it is important to evaluate for prostate perfusion and collateral vessels that are dangerous to embolize. Cone-beam CT can help identify vessels that feed non-target tissues. In this companion case, cone beam CT in the presumed prostatic artery revealed enhancement of the rectum more consistent with a middle rectal artery, and embolization was not performed.
Once the catheter was positioned in the prostatic artery, 100 ug of nitroglycerin were administered to reduce vasospasm and the left prostatic artery was embolized to stasis with microparticles. Of note, a technique known as PErFecTED (Proximal Embolization First, Then Embolize Distal) is popular among some operators in which proximal embolization of the prostatic arteries is performed first, followed by wedging of the microcatheter into the intraprostatic arteries where additional embolization is performed. Some evidence suggests this technique increases prostate ischemia and infarction.
The right internal iliac artery was then selected using the RBT catheter. DSA was performed. The indicated artery was catheterized. Cone beam CT was then performed.
Cone beam CT demonstrated mild enhancement of the prostatic capsule as well as a region of the rectum, suggesting the vessel was a middle rectal artery. Embolization was not performed to minimize damage to the rectum. The prostatic artery was selected and cone beam CT was performed.
The prostatic artery was selected and cone beam CT was performCone beam CT performed with catheter tip in the prostatic artery revealed supply to the prostate. As illustrated in this case, cone beam CT can help reveal collateral flow to the prostate as well as assess for off target embolization. Nitroglycerin was administered and the right prostatic artery was embolized to stasis with microparticles.
In terms of efficacy, the improvement in IPSS following PAE ranges from 11.2 to 18 points, and the improvement in quality of life (QoL) scores ranges from 1.9 to 4.7 points. There is clinical success in ~82% of patients from 1-3 years after PAE, and in ~76% of patients from 3-6.5 years.
Compared to the most common surgical option, TURP and PAE have similar reductions in subjective measures like IPSS and QoL. However, TURP tends to have greater improvements in objective metrics such as prostate volume, post-void residuals, and maximum urinary flow rate. PAE on the other hand tends to have fewer complications although greater recurrence of symptoms.
Learn more
Case contributed by Drs. Benjie Smith, J.C. Panagides, Amanda Rigas, and Andrew Picel from Stanford University






